This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
In 2017 the first immuno-oncology cell therapies, known as chimeric antigen receptor T cells, or CAR T, were approved by the U.S. Food and Drug Administration. Immuno-oncology cell therapy is a field that leverages the immune system by modifying, and thereby enhancing, immune cells to target cancer. It accomplishes this by interdicting pathways that maintain checks and balances on cellular elements of the immune system, thereby disrupting the tolerance of the body to the growth and spread of cancer.
CAR T therapies have had unprecedented success in blood cancers, such as certain leukemias and lymphomas. They have shown high response rates and redefined the treatment of patients who have exhausted other options. Their therapeutic success relies on an antibody fragment that binds to a surface protein on leukemias and lymphomas; one such protein is known as CD19. The antibody fragment is linked to stimulatory and signaling molecules that fire on binding of the antibody with the CD19 molecule, thereby activating the T cells and making them destroy the cancer cell.
Solid Tumor Challenges
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
CAR T therapies have shown limited success in solid tumors because they do not typically express a molecule on their surface that is unique to the tumor and not common to normal tissue. Coupled with the complex matrix in which cancer cells grow, this makes it challenging to develop cellular therapies for solid tumors.
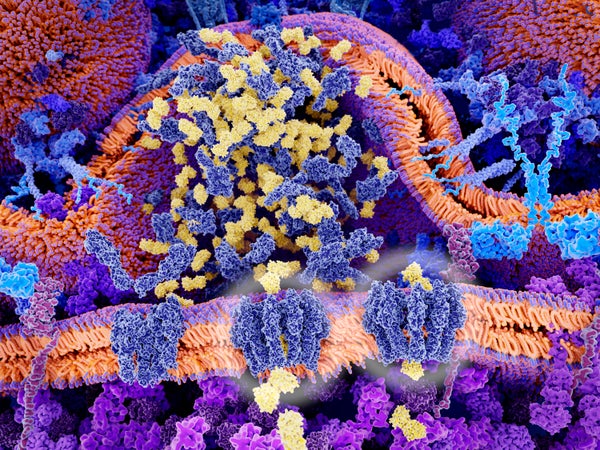
One way to overcome this challenge is to target proteins expressed inside the cell rather than large cell-surface proteins. This kind of immune response involves the activation of T cells against a part of an internal protein that the T cells see as foreign. These protein fragments, known as peptides, dock with protein structures on the cell surface known as major histocompatibility antigens (MHCs), which are the cellular network that governs the presentation of self versus nonself peptides and lets T cells distinguish friend from foe.
T cells are some of the “surveyors and assassins” of the immune system. They have T cell receptors (TCRs) on their surface, and they circulate through the body, binding foreign peptides on the surface of cells that are infected by foreign organisms such as viruses and bacteria. When a cell is infected, bits of that organism’s protein make it to the surface, docking with the right MHC. Surveying T cells can see these proteins through their TCRs and kill them to prevent propagation of the infection.
Yet cancer cells have proteins that look similar to the body’s own, not like foreign proteins, which fosters an ability to evade the immune system. This makes it difficult to effectively target tumors with our body’s own naturally occurring TCRs. When cancer cells develop mutations, they may present novel, aberrant peptides, but often the malignant cell and other elements of the tumor dampen the T cell response by interfering with the molecular network that regulates how T cells function. The unraveling of some of the proteins that regulate T cell function against tumor cells resulted in two scientists sharing the 2018 Nobel Prize in Physiology or Medicine.
The Potential of Enhanced Receptors
Companies are now exploring how to enhance the body’s naturally occurring TCRs to target solid tumors. Engineering TCRs to have optimal affinity for the docking peptide enables the receptors to more easily identify proteins from cancer cells that would otherwise not be recognized as foreign.
These engineered TCRs can be put into a patient’s own T cells, which are then returned to the patient. These newly enhanced T cells can kill tumors, multiply and attack more cancer cells than a patient’s naturally occurring T cells.
Biopharmaceutical company Adaptimmune uses its unique SPEAR (specific peptide enhanced affinity receptor) T cell platform to engineer TCRs that can recognize cancer proteins on solid tumors.
Future Immuno-Oncology
There is still more to come from the immuno-oncology cell therapy field with respect to utilizing TCRs, given that many solid tumors recur and become incurable. This is why Adaptimmune is conducting clinical trials with multiple engineered TCRs across a broad range of solid tumors. The company is also investigating next-generation TCRs armed with molecules to further improve the engineered T cells’ ability to target and destroy solid tumors. These enhanced approaches will likely lead to longer-lasting antitumor responses.
Patients in dire need of novel treatment options are the driving force pushing Adaptimmune and many companies in the life sciences industry to continue the quest to eradicate metastatic cancer. The field has come a long way, and its potential appears boundless as scientists unravel the intricate interplay between cancer and anticancer immunity.
Update: Since this article was published three years ago, Adaptimmune has made great progress with its engineered SPEAR T cells for solid tumors. Later in 2022 we plan to file a biologics license application request to the FDA for approval of our lead product, afamitresgene autoleucel (afami-cel), for the treatment of synovial sarcoma. Afami-cel uses an engineered TCR to target the cancer/testis antigen MAGE-A4. A phase 2 trial of the therapy has shown a response rate of 36 percent in synovial sarcoma. This rare and difficult-to-treat cancer presents a high unmet medical need, for which afami-cel is a potential game changer.
We have also launched several trials of next-generation SPEAR T cells targeting MAGE-A4. An early trial has shown promising initial responses in synovial sarcoma and in esophagogastric junction, ovarian, head and neck, and bladder cancers. Based on these responses, we initiated a late-phase trial for gastroesophageal cancers, and we plan to launch one for ovarian cancer later this year.