This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
It was probably only a matter of time until someone connected the dots.
Prions – infectious proteins -- had turned up in the eyes of victims of prion diseases.
Infected donor corneas had transmitted prion disease to recipients on at least a few occasions.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
And often, patients who later turn out to be infected with prions have eye trouble for which they seek medical attention and testing before they are aware they are infected.
What if … ?
The possibility was horrifying. But it demanded investigation.
Prions are proteins, and, as every biology student knows, proteins are dependent on DNA and RNA for their existence. Yet prions have stumbled upon a way to beself-replicatingnonetheless. Their diseased shape induces proteins of similar sequence but healthy shape – found abundantly in all nervous tissue -- to misfold when they collide with a prion. Now they are infectious too, part of a relentless and lethal domino effect.
The diseases they cause are grim. Mad Cow Disease is the most famous, but kuru also possesses a certain notoriety thanks to its unorthodox mode of transmission. Although uncommon, prion diseases are incurable and bring dementia swiftly followed by death. In the case of spontaneous Creutzfeldt-Jakob Disease (sCJD), the most common prion disease, half of patients are dead within six months of symptom onset. That figure reaches 95% within a year. In a particularly vexing twist, prions are also nearly impervious to destruction, even when attacked using a strenuous combination of disinfectants, heat, and pressure.
As you can imagine, this makes prions difficult to eliminate from infected tissues and equipment. In addition to corneal transplants, sCJD has also been transmitted by transplants of brain tissue called dura mater, growth hormone from cadavers, and perhaps most worryingly, neurosurgical instruments. So any method that might throw prions into the path of uninfected people deserves scrutiny.
Enter the study published in November in the journal mBio by a team of American scientists that found the eyes of human prion victims are loaded with infectious particles even before they have begun to exhibit symptoms. Further, these particles are present on the surface of their corneas, the covering of the eye. 100% of the eyes of 11 sCJD victims who donated their bodies for study were seeded throughout with prions. 100% of their corneas contained prion seeding of a “low to moderate” degree. Because the cornea is enervated, the prions, which prey on proteins found in neurons, may be reaching the surface via these tiny neural conduits.
The retina – the light sensing layer at the back of the eye -- was most densely packed with prions in the inner and outer plexiform layers. They were easily visible in tissue stains.
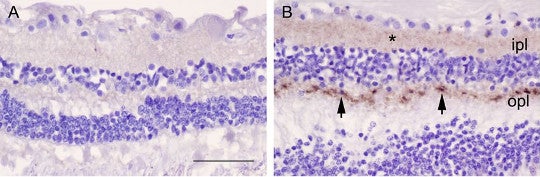
Normal retina (left) and diseased retina (right). Prions visible as a brownish stain in the inner and outer plexiform layers. Credit: Orrù et al. 2018
In half of the 11 cases, the concentration of prions in the retina approached levels found in the brain, the epicenter of prion activity.
On the plus side, this finding, combined with the relative ease of assessing the retina, suggests a new target for traditionally tricky CJD diagnosis by non-invasive methods as electroretinograms.
On the other hand, all remaining implications are disturbing. It’s unknown how early in the disease process prions appear in the eyes of humans, but in rodents, they are present prior to the onset of disease. About 40% of sCJD patients develop eye-related symptoms serious enough to warrant a consultation with an ophthalmologist. Somwhere between a quarter and a half go blind.
Undiagnosed CJD patients may seek testing. And the diagnostic equipment used to test them may then become contaminated, the authors write. They recommend single-use instruments or the adoption of new decontamination procedures for opthalmological equipment with better effectiveness on prions.
Meanwhile, corneal transplants are becoming increasingly popular worldwide. According to the authors, 185,576 were performed in 116 countries in 2012, a new high. The United States leads the world per capita, with 64,000 performed each year. The authors further recommend speeding and perfecting the development of synthetic corneas to reduce the need for donor corneas.
But there are yet more worrying implications of these findings.
As I wrote about at this blog earlier this year, there is a growing uneasiness that the clumping proteins associated with some of the most common and deadly neurodegenerative diseases behave in ways that are uncomfortably similar to prions.
One question suggested by this research is whether the eyes of Alzheimer’s and Parkinson’s patients are likewise filled with amyloid-beta, alpha-synuclein, and tau, and if that is the case, if the accumulation of those proteins in eyes might be exploited to aid diagnosis, a notoriously tricky proposition for these diseases.
Another is – and I am entering deep speculative territory here, as in, no one actually qualified to render an opinion on this has said it, I’m just putting two and two together in my head -- whether ophthalmological equipment could act as a vector for those diseases, as surgical equipment has already been hypothesized to do.
Don’t skip your eye exam. But given the seriousness of the stakes, I hope that someone out there is investigating these hypotheses. Yes, the odds are low. But the stakes are very, very high.
Reference
Orrù, Christina D., Katrin Soldau, Christian Cordano, Jorge Llibre-Guerra, Ari J. Green, Henry Sanchez, Bradley R. Groveman et al. "Prion Seeds Distribute throughout the Eyes of Sporadic Creutzfeldt-Jakob Disease Patients." mBio 9, no. 6 (2018): e02095-18.