This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
Innovation has been the driving force of excellence in American medicine. From development of anesthesia to heart bypass, innovation in treatment modalities has saved millions of lives across the country—and the world. What is often not studied thoroughly is whether integration of novel medical innovations increases the cost burden on the health care system. More importantly, what is the role of patients—if any—in adoption of these innovations?
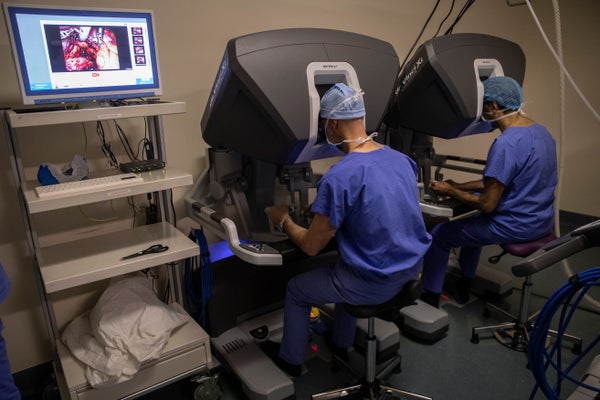
For instance, robotic surgery is a technology that allows doctors to perform complex procedures with more precision. It has seen an exponential increase in adoption across clinical specialties in the past two decades. This adoption is driven largely by specific advantages associated with the robotic approach: shorter hospital stay, less blood loss, and lower pain medication requirements.
However, the evidence that robotic surgery leads to better outcomes remains ambiguous. This unchecked increase in adoption has even led the FDA to issue a warning to not use robotic surgery for certain procedures, given a lack of evidence on risks and benefits.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
This is especially pertinent in the current political climate because U.S. national health care spending is on an increasingly unsustainable course. In 2018, the national health expenditure (NHE) was $11,172 per person. The year before, administrative burden cost $812 billion, according to a revealing recent study in Annals of Internal Medicine. These grim numbers have led to a renewed focus on investing in value-based health care delivery models, that emphasize improving the outcomes of care while reducing costs.
In a study published recently, our research team at Brigham and Women’s hospital sought to understand whether a positive value proposition for the patient played a role in adoption of robotic cancer surgery. We started with a simple question: Does robotic surgery present a more affordable option from a patient’s perspective?
Previous investigations looking at this question relied on understanding total health care expenditure—which, while important, is not a good marker for value proposition for the patient. For patients, what often matters more is how much they are paying out of pocket, because this is usually the expense that is “visible” to them. We reasoned that this expense was more relevant for understating the role of patients in adoption of new medical technologies.
Turns out, the answer to this question is more complicated than previously thought. To start with, our analysis reveals that for five major cancer surgery procedures (for disease in the prostate, uterus, colon and kidney), robotic cancer surgery was associated with lower out-of-pocket costs compared to open surgery—presenting a more affordable option from a patient’s perspective.
Our study was an economic analysis of 15,893 patients who underwent one of the five major surgical procedures, using deidentified insurance claims for 1.9 million enrollees from January 1, 2012, to December 31, 2017. Interestingly, we found that patients undergoing a robotic approach for the removal of uterus were older than those undergoing the open approach; and patients undergoing open approach for kidney cancer had more coexisting diseases than those undergoing the robotic approach—revealing that the decision to choose one of these options is still primarily driven by clinical considerations.
To frame our findings within the context of current literature, we conducted an extensive review of evidence to understand why out-of-pocket expenses would be lower for a more advanced procedure such as robotic surgery. Our review reveals that three major economic forces could be driving the adoption of robotic surgery: direct advertising to patients, centralization of care, and integration of the robotic platform in surgical training programs.
To begin with, while profitability remains an important motivator for rapidly adopting robotic surgery, a key contributor as to why hospitals are willing to absorb the high upfront costs of robotic surgery is patient demand. We already knew that direct-to-consumer advertising (DTCA) of robotic surgery increases demand. It is possible that this higher demand is influencing hospitals to offer robotic surgery in order to retain a competitive advantage. Our finding of significantly lower out-of-pocket costs associated with the robotic approach are likely to compound this trend.
Another reason for rapid adoption of robotic surgery has been the centralization of surgical procedures. Current evidence suggests that institutions acquiring the robot have seen a dramatic rise in their surgical volume, while those who did not, experience the opposite phenomenon. It has also been reported that high-volume surgeons in the U.S. at teaching and large-sized hospitals have swiftly adopted a robotic approach.
Lastly, rapid adoption of robots could be a result of changes in the surgical residency training programs. Recent evidence points to residency programs increasingly training their residents in operating on robotic platforms, highlighting that, after residency, trainees may be better equipped with using this option. And since high-volume centers are more likely to use a robotic platform—and teaching hospitals tend to be high-volume centers—these trends in adoption are likely to continue expanding.
To be sure, our findings should be interpreted carefully, as our analyses did not account for procurement or maintenance of the expensive robotic platforms (costs could run in millions of U.S. dollars). However, since we relied on an accepted methodology—and calculated out-of-pocket expenses using cost information from inpatient care, outpatient care and outpatient pharmacy during the perioperative and postoperative periods—we do believe the estimates are precise.
These findings provide useful insights for policy makers on how the health care system promotes adoption and dissemination of innovative medical technologies and the importance of understanding the patient’s perspective. For far too long, policy makers have focused on simplistic reasoning—profitability, greed—to describe the rapid adoption of novel medical technologies in clinical practice. Our findings provide the foundation for future research on these issues and reveal why designing policy solutions that lead to steady adoption will require a systems-level thinking.