This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
The World Health Organization recently proposed a new 10+1 initiative for malaria control and elimination that targets 10 of the African countries (plus India) that host 70 percent of global cases.
While this initiative is promising, it is missing an important component: genomic surveillance. Drug resistance threatens all the progress made so far against malaria, but genomic surveillance can detect drug resistance years before the first warning signs appear in clinics. It can answer important questions about how resistance emerges and spreads, and it can help control the balance of interventions, preserve the useful life of already existing drugs, and ensure effective treatment.
On this World Malaria Day, I call on the WHO, global health partners and the malaria community to incorporate mandatory genomic surveillance of malaria parasite by making it a major intervention in countries that have the highest malaria burden. This genomic information can help country malaria control programs use quality data sets for regular monitoring of drug resistance, to provide evidence-based decision making around malaria policy, and to manage the spread of resistance in country.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The African countries most affected by malaria all had a first line drug that ended up becoming resistant. In the 1990s, chloroquine was the first line treatment, but malaria parasites grew resistant to it. This drug was then changed to sulfadoxine/pyrimethamine in the early 2000’s and resistance occurred. Now, malaria parasites are becoming resistant to the current first line drug Artemisinin Combination Therapy (ACT’s). Artemisinin resistance is conferred by a gene known as Kelch13, located in the propeller region of Chromosome 13.
Whilst mutation in this gene has occurred in Southeast Asia and is spreading around the region, there are fears it will spread to Africa, like it did for the drugs before it. The more drugs we use to treat malaria parasites, the more resistant they become due to selective pressure, which creates the pre-conditions for resistance to occur. Since we know this biological response from the parasite is inevitable, we should put in place measures to track these changes down when they occur as this would help us prevent the spread, investigate emergence and subsequently preserve the efficacy of the current first line antimalaria treatment.
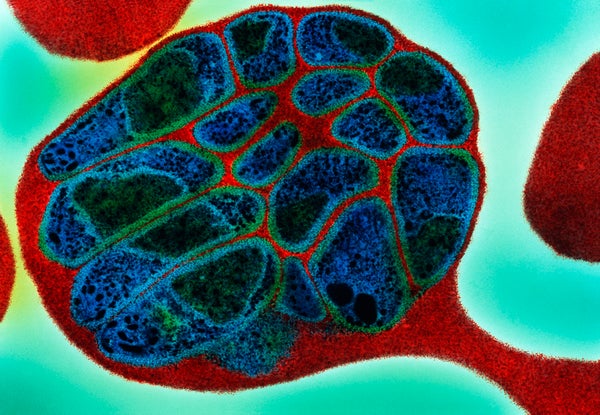
With advances in genomic technology, scientists have been able to analyse malaria parasites from the patients carrying the disease, to the mosquitoes transmitting the disease and has become a source of relevant information for both drug resistance and insecticide resistance. Research shows that genomic surveillance has helped us understand how different mosquito species arise and how they transmit malaria to humans, which in turn has led to a better targeting of interventions as vectorial capacity is better understood.
It has enabled better understanding of changing transmission intensity, parasite gene flow including drug resistant genes, and has aided in quantifying the risks of importing malaria from a country with malaria burden. However, most of the work carried our using genomic surveillance as a tool, have mostly occurred within the realm of research, with only a few examples of its application in the field where malaria burden remains high.
Genomic surveillance has been used in countries that have eliminated malaria to prevent resurgence and in countries that are in malaria elimination phase. It shouldn’t be any different for the African countries that have the highest malaria burden. Lessons learned from polio show that genomic surveillance played a huge role in controlling the infection. Public health officials have been able to use quality data to understand where this virus emerged from, map the transmission network and understand where to direct their vaccination efforts.
It is time genomic surveillance moves from mainly academic research into the field where malaria deaths occur. I propose the WHO incorporate a new “took kit” that includes malaria genomics to eradication plans. It should be integrated into large-scale public health interventions that will provide valuable information for improving operational decisions made by the national malaria programs of African countries that make up the 10+1 initiative.