This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
In 2022 an estimated 1.9 million new cancer cases will be diagnosed in the U.S., the equivalent of some 5,190 new cases each day. Furthermore, approximately 600,000 Americans are predicted to die of cancer—a staggering 1,670 deaths a day.
As the second most common cause of death in the U.S., exceeded only by heart disease, cancer places a tremendous burden on individuals, families and our society as a whole. The Medical Care Costs Associated with Cancer Survivorship in the United States report estimates that the direct medical costs for cancer in the U.S. in 2021 were an overwhelming $208.9 billion.
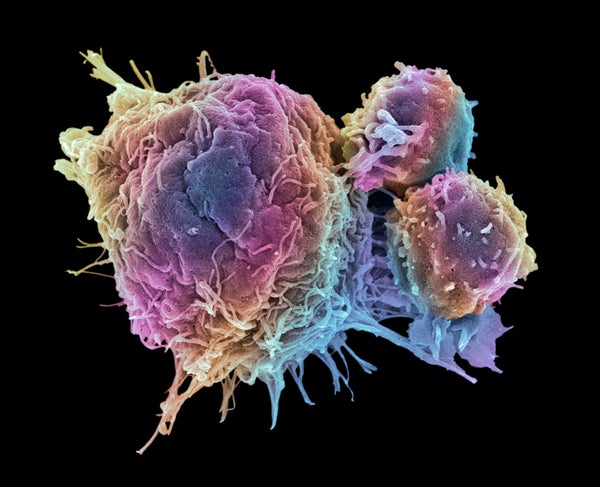
Over the past decade significant advances in research, education, early-detection methods and treatment have boosted cancer survival rates, and new therapies continue to be developed. The recent introduction of cancer immunotherapies, in particular those based on immune checkpoint inhibitors, has created a paradigm shift in clinical oncology. These drugs work by unleashing the body’s own immune responses to promote elimination of cancer cells.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
While traditional therapies such as chemotherapy and radiation are often used as a first-line treatment to fight cancer, immunotherapy has been gaining popularity with the support of promising research, clinical trials and new reimbursement from the Centers for Medicare and Medicaid services. In fact, a recent analysis shows that hospitals are investing more in cancer immunotherapies, with researchers finding a 199 percent rise in spending on immunotherapies used to treat small-cell lung cancer during the first three quarters of 2019, compared with the same period in 2018. Moreover, first-line immunotherapy, either alone or in combination with chemotherapy, is considered the standard of care for patients with non-small-cell lung cancer.
Although tremendous progress has been made with immunotherapy modalities, today only a small percentage of patients are benefiting from such therapies. It is estimated that 43.63 percent of U.S. cancer patients are eligible for checkpoint inhibitor immunotherapy, and on average, only 12.5 percent will respond. These are best-case estimates, however, and additional studies for several of these drugs have failed to show improvement in overall survival or progression-free survival.
At the same time, the high cost of immunotherapy ($30,000 to $300,000 per year for an individual patient) and the risk of developing immune-related adverse events place pressure on the health system to prescribe such therapies to only those patients who are most likely to benefit. And robust methods to identify appropriate candidates for immunotherapy are still lacking.
From the pharmaceutical industry’s perspective, the inability to predict which patients will benefit from immunotherapy has resulted in the recent failure of several major clinical trials. For these reasons, identifying appropriate candidates for immunotherapy is critical for maximizing clinical benefit, avoiding unnecessary toxicities and reducing costs.
It is time to rethink the way we approach immunotherapy to benefit even more patients and their loved ones, while considering the financial realities on the ground. With the recent rise of artificial-intelligence and machine-learning tools to analyze complicated medical data, we now have the opportunity to profile patients earlier on in the treatment process to gain a new level of understanding that will ensure that precious time won’t be lost on a therapy that won’t have a positive impact or any impact at all.
If a patient’s response to a given treatment plan can be predicted before it even begins, costs will be saved, and the person can be spared from unnecessary side effects.
Host Response
Although many cancer treatments initially show positive results, eventual resistance, characterized by tumor relapse or spread, is common. Traditionally, studies investigating tumor aggressiveness and resistance to therapy have focused on tumor-related features such as genetic and epigenetic changes that either accumulate over time or exist from an early stage. But this is only part of the picture.
Looking beyond the tumor to see the actual patient, or “host,” adds an important layer of information. It is now becoming clear that the physiological reactions of the host to the treatment, collectively known as the host response, ultimately influence tumor behavior, often in favor of tumor growth and spread. For several years researchers have been investigating how an individual’s unique host response to a variety of cancer therapies may promote therapy resistance and worsen the outcome, as summarized in recent scientific reviews.
In a practical sense, the host response to any given cancer therapy can be monitored in real time by analyzing a broad range of selected proteins in the patient’s plasma. This analysis, done before treatment begins, provides insight into how the person might respond, along with prognostic evaluation and profiling of resistance mechanisms of the tumor-therapy-host triad. How does it work? An analysis of proteins that are differentially expressed between patients that respond and those who don’t is performed. Machine-learning tools, combined with bioinformatics and biological analysis, then identify resistance-associated proteins, resistance pathway networks and associated drugs, or drugs in clinical development that may address resistance.
With this analysis, the platform deals with three clinical questions: 1. Will the patient respond? 2. Why does resistance occur? 3. What might be the next step in treatment? Answering these questions even before treatment begins provides clinicians and their patients with a layer of information that simply doesn’t currently exist. This approach holds the potential to support clinical decision-making, allowing for data-based, personalized choices of different combinations of immunotherapy and, in the best scenario, improved outcomes.
In addition, this technology allows us to identify potential drug targets and drug combinations and possible development of companion diagnostics. Using proteomics analysis in biomarker discovery and early detection in cancer is a rapidly growing field that some believe is the next quantum leap in precision medicine.
As an example, consider a group of non-small-cell lung cancer patients who are receiving standard-of-care, “one size fits all” immunotherapy protocols. To date, we do not have biomarkers that can discern accurately between patients who will benefit from a certain drug or treatment combination. Furthermore, in the next couple of years we are going to see even more combinations of immunotherapy approved (there are more than 30 currently ongoing phase 3 clinical trials looking at different combinations of immunotherapy). Choosing among these options without biomarkers to guide the choice is impossible, and not choosing but rather using trial and error is simply unacceptable. With the new biomarker platforms developed today, including host-response profiling, new clinical insights will be available for patients and clinicians before they even begin treatment, changing the game completely.
Protein-based biomarker platforms identify and measure biological processes that fuel tumor progression and, accordingly, are highly predictive of treatment outcome. By detecting these interactions before treatment even begins, rather than later in the cycle, physicians and oncologists can better plan and adjust treatments that will be effective on the individual level. With a focus on patients diagnosed with advanced stages of melanoma or non-small-cell lung cancer receiving immunotherapy, clinical trials have shown this method of pretreatment analysis on host response to have high accuracy. These results are statistically and clinically significant, giving us great hope for the future of precision oncology.
With the tools we have in hand, the future of cancer treatment is bright. The American Society of Clinical Oncology has recognized the need for identifying strategies that better predict response to immunotherapy as one of the top nine research priorities to accelerate progress against cancer. Host-response analysis takes us a crucial step forward in achieving this goal.
As we head further into the decade, host-response profiling for cancer therapy will play a growing role in precision medicine for oncology. The value that pretreatment validation will provide, both to cancer patients and to their clinicians, is invaluable. We can now be empowered with a level of knowledge that until now was nonexistent. Understanding the likely patient response for a full 12 months before treatment initiation, combined with insights on resistance-associated pathways and proteins, should allow physicians to make critical clinical decisions earlier, all based on personalized patient data.