This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
Millions in the U.S. take statins like Lipitor for lowering cholesterol to prevent or treat heart disease. The success of statins has planted the idea of taking a similar pre-emptive strategy to meet the desperate need for new Alzheimer’s drugs.
In a recent edition of Science Advances, researchers from three European universities offered up a new approach to developing preventive drugs based on an understanding of a key biochemical process that precipitates Alzheimer's. The team then used this knowledge to track down an FDA-approved drug that seems to halt the pathology, which they labeled a “neurostatin.”
The work is earlier than early stage. It was carried out using genetically engineered roundworms, not even mice. And the drug, an anticancer agent called bexarotene, has a side effect of raising lipids called triglycerides that would probably make it unsuited for long-term use as a statin-like drug.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Bexarotene, what’s more, failed to meet its objectives of stopping or slowing the disease in two small clinical trials and, if that weren’t enough, it has trouble getting through the blood-brain barrier. One newspaper covering the study trumpeted the headline: “The Pill That Could Stop Millions Getting Dementia.” Right now, that is not even wishful thinking, though the story in the Daily Mail probably did meet its primary clinical endpoint of getting lots of clicks.
So what, if anything, is good about all this? The team from the University of Cambridge, Lund University and the University of Groningen used detailed math to model how the disease process unfolds to optimize the prospects of finding drug candidates that bring to a halt the molecular havoc wrought by dementia.
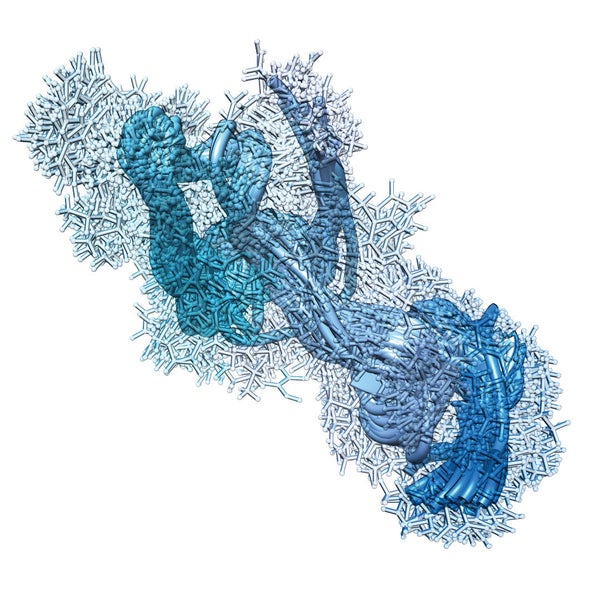
An autopsy of the Alzheimer’s brain turns up clumps of peptides that hinder communication among brain cells, and ultimately abet in the destruction of neurons. The researchers’ model reveals the rate at which various processes in the aggregation reaction evolve—in other words, the chemical kinetics that determine when the peptides combine, or "self-assemble," as chemists like to say.
Using information about aggregation rates, the researchers went on to look for potential drug candidates that would do their job by bollixing up the precise timing that the amyloid-beta peptide implicated in the disease requires to form toxic garbage heaps.
Tracing the kinetics allows for the creation of a minute chronology of debris buildup: when single amyloid-betamolecules first stick together and when budding aggregates, or oligomers, grow to form tiny fibers (fibrils) that cluster together. That timeline continues as fibrils speed aggregation by catalyzing the formation of still more oligomers on their surfaces.
Measurement of these steps can be matched to clinical progression of the disease, either before or after a person experiences cognitive problems. Having this information may allow design of drugs to either prevent disease—a hypothesized neurostatin—or to treat it once a diagnosis has been made."
Michele Vendruscolo of the University of Cambridge, the paper’s senior author, says that the team’s model showed that bexarotene would work at the very earliest stage when the amyloid-betapeptides formed oligomers, but would not do so as the pathology continued. Alzheimer roundworms treated with bexarotene continued to move about normally, whereas untreated ones slowed their paces. (Unsuccessful human clinical trials of bexarotene were premised on a different mechanism of action in which the drug would remove the amyloid peptides from the brain at a later disease stage.)
Even as a preventive, ingesting bexarotene might be futile because it has trouble getting into the brain—and it also raises triglycerides. Vendruscolo emphasized that the study’s success did not hinge on tagging bexarotene as possible Alzheimer’s medicine. Rather, the ability to model the kinetics of amyloid-beta—and then use that knowledge to look for potential drugs—paves the way for a general-purpose Alzheimer’s drug discovery machine. In fact, the same techniques might be used for modeling other molecules involved in Alzheimer's pathology—or doing the same for other neurodegenerative diseases. “Bexarotene is a proof of principle, Vendruscolo says, “but, in fact, we already have other compounds that act in the same way. Some of the potential neurostatins are more potent than bexarotene, he notes, adding: “Bexarotene may or may not become an effective preventive drug but we already have better compounds.”
The response to the study was cautious, but by no means dismissive. James Hendrix of the Alzheimer’s Association says that anti-aggregation drugs might work along with others under development to remove amyloid-beta, an approach to treating neurological disease reminiscent of drug cocktails for HIV or cancer. Stopping the peptide pileup could be an integral element in combination therapies. “I think that it’s important to look at this strategy as another way to attack the disease," Hendrix says.
Harry LeVine, a professor at the University of Kentucky, remembers analyzing the kinetic reactions of amyloid-beta when he worked in drug development at Parke-Davis (now a subsidiary of Pfizer). His laboratory, instead of doing a single overall analysis, the approach documented in the Science Advances study, chose to look at kinetics in a series of steps. A possible drug compound would undergo separate tests to determine how it interacted with amyloid-betaat each stage of aggregation—nucleation (first entanglement), oligomers, fibrils, etcetera. That way, subtle effects or technical artifacts in the data might be more apparent. “It’s a very complicated system,” LeVine says. A lot of things can happen so interpreting it can be difficult.” (The researchers of the Sciences Advances paper contend that all of the steps need to be modeled together to suss out the aggregation process.)
LeVine says that the pharmaceutical industry was interested in developing anti-aggregation agents, but has since shied away. “There’s a number of compounds out there that supposedly blocked aggregation that when they were run through clinical trials they didn't show effects,” he says. “Now there are a whole bunch of reasons why that might be. Pharma isn’t necessarily interested in tracking down all those reasons.”
Maybe they should show more interest. Pharma still has deep expertise in finding compounds that interfere with the kinetics of a disease-related biochemical process. That knowledge is sorely needed. By one estimate, the number of Alzheimer’s cases are expected to balloon from the current 40 million worldwide to reach 130 million in the next 35 years.
Getting on board would be a departure from the status quo of developing the drug du jour—yet another hepatitis C compound, for instance. Yes, the risks are high. But the Science Advances study shows the potential of following the amyloid. And the rewards, if just one compound succeeds in slowing Alzheimer’s relentless progression, would be a blockbuster that would match Lipitor or any other of the highest-grossing drugs in the industry’s history.