This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
Scientists will never find a single gene for depression—nor two, nor 20. But among the 20,000 human genes and the hundreds of thousands of proteins and molecules that switch on those genes or regulate their activity in some way, there are clues that point to the roots of depression. Tools to identify biological pathways that are instrumental in either inducing depression or protecting against it have recently debuted—and hold the promise of providing leads for new drug therapies for psychiatric and neurological diseases.
A recent paper in the journal Neuron illustrates both the dazzling complexity of this approach and the ability of these techniques to pinpoint key genes that may play a role in governing depression. Scientific American talked with the senior author on the paper—neuroscientist Eric Nestler from the Icahn School of Medicine at Mt. Sinai in New York. Nestler spoke about the potential of this research to break the logjam in pharmaceutical research that has impeded development of drugs to treat brain disorders.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Scientific American: The first years in the war on cancer met with a tremendous amount of frustration. Things look like they're improving somewhat now for cancer. Do you anticipate a similar trajectory may occur in neuroscience for psychiatric disorders?
Eric Nestler: I do. I just think it will take longer. I was in medical school 35 years ago when the idea that identifying a person's specific pathophysiology was put forward as a means of directing treatment of cancer. We're now three decades later finally seeing the day when that’s happening. I definitely think the same will occur for major brain disorders. The brain is just more complicated and the disorders are more complicated so it will take longer.
SA: Do you have any estimates of how long it might take?
EN: I don't think it will be 30 years because we’ve learned a lot from cancer and other fields like immunology. That will guide us and teach us as we make progress for the brain so I would say between five or 10 years. There are already insights—specific genes and biochemical pathways—that have been identified now for brain disorders that are being followed up on. If we get lucky and some of those prove to be useful, we can start to see some clinical advances within about five years.
SA: There have been a lot of genetic studies that have looked for links between genes and psychiatric disorders but they turn up hundreds of genes of interest. How do you actually proceed to use that information to do something useful to both understand disease and to treat it?
EN: This is a major question of our time. One approach is to determine how differences in hundreds of genes would affect key biochemical pathways inside the brain. Although there are hundreds of genes, the expectation is that there's just a handful of altered biochemical pathways. Now if we could find those pathways and how they're altered and figure out ways to reverse those changes, we might be able to come up with new therapeutics. That is our working hypothesis now.
SA: Can you take information from one of these large genetic studies of recent years and use a technique to find either a key gene or pathway?
EN: Doing that is complicated because we're dealing with literally tens of thousands of gene products—proteins or RNAs (the latter are molecules that, along with DNA, encode the making of proteins). And so we must sift through how a few hundred out of tens of thousands of these gene products are altered. How they influence biochemical pathways is a complicated process in and of itself. But this process is tractable and it is work that can be done now.
SA: Aren’t you using multiple techniques to try to deal with this complexity?
EN: We use several approaches. First we identify the tens of thousands of RNAs present in different brain areas and put that information together with direct measures of how different brain areas function abnormally in an animal model of depression. It's an effort to help us determine which of many thousands of these gene products would be the most important to study. The real challenge right now is one of bandwidth. If you find hundreds or thousands of genes, how do you know which ones are the best to study first?
SA: How do you?
EN: It is overwhelming at first, but we use several statistical approaches and overlay different data sets on one another. Genes that come up repeatedly in multiple models in multiple ways from multiple angles are more likely to be important than others.
SA: What are one or two examples of the techniques that you have now that you didn't say 10 or 20 years ago that would have made this research impossible back then?
EN: Right now it's possible to identify all of the gene products expressed in a given brain area or even within a single type of cell within a given brain area. That couldn't have been done years ago. Then we can use various tools to identify the genes that are most dramatically regulated in those cells in mice exposed to chronic social stress. And then we identify several specific genes that come up as being important in overlapping approaches and study them directly.
We can have a single gene make more protein than normal or turn that gene off within a targeted cell type within the brain. Wecan thereby see whether turning that gene expression up or down mimics or reverses depression-like behavior in an animal model. Then we can understand how that gene product alters the functioning of the cell. Does it excite the cell, make it more active or make it less active? Next, we can use optogenetics tools that can directly manipulate the activity of that given cell type in an awake, behaving animal. So for the first time it's possible for the field to start out with genetic methods and bring them all the way forward to see how nerve cells are functioning within the brain in a live animal to influence depression-related behaviors.
SA: What tools would you still really like to have if you could?
EN: I think the main advances that are still needed now are to find ways to make it easier to manipulate individual cell types. The ability exists, we just need to expand the tools available. The second thing is the ability to manipulate several genes at once. Right now the tools that we and others use enable manipulating only a single gene at a time. It would be very nice to go into an experimental animal and manipulate multiple genes at one time. New gene-editing techniques make it possible theoretically to do that, but it's still not straightforward, particularly in brain.
SA: What did you do in the experiment reported in the Neuron paper?
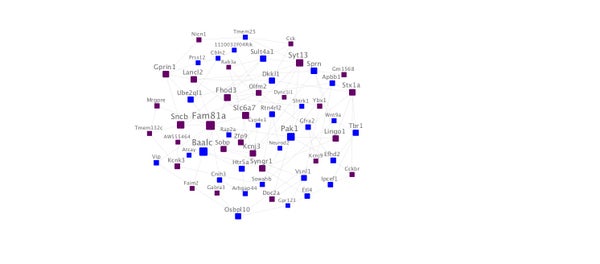
EN: Rosemary Bagot, the study’s first author, and our colleagues used these methods to identify the most important genes in a mouse depression model and then developed tools to either overexpress a given gene of interest or to knock it out. We then studied the consequences of those manipulations on behavior. One of the most interesting genes that we found by looking with statistical tools through 20,000 genes was Dkkl1. The gene is known to be involved in signaling in a basic biochemical pathway called Wnt inside of cells. We identified the brain area where this gene seemed to be playing the most important role and that was the hippocampus (an area important for learning, memory and emotional behavior). We thus overexpressed Dkkl1 (encoded more of its protein than normal) in the hippocampus and studied the effects on behavior and gene expression.
Our molecular data suggested that Dkkl1 is a very important hub gene that regulates other key genes and we showed that overexpressing Dkkl1 in the hippocampus was enough to make mice susceptible to stress and to induce depression-like behavior. Dkkl1 overexpression also selectively regulated genes that it was predicted to regulate in our data sets. This illustrates the ability go from using very basic statistical methods for gene discovery all the way to finding a new gene never studied before in models of depression-like phenomena.
SA: Would you say that this approach could be used in studying other psychiatric diseases as well?
EN: Yes, most definitely. And, in fact, efforts are under way by us and others to do this kind of work in several other syndromes such as autism, schizophrenia, bipolar disorder, drug abuse and so on.
SA: What will be the potential payoff both in understanding depression and in developing drugs to treat it?
EN: Right now we still have very limited understanding of the molecular underpinnings of depression. So studies like this can identify a more complete list of genes and biochemical pathways involved in depression. The work now provides a template that can guide drug discovery efforts. If Dkkl1 is in a depression-related pathway, we can ask how we might affect this pathway in a way that would be predicted to produce an antidepressant response?
SA: How would a drug produced in this way potentially be better than the antidepressants we have now?
EN: All of the antidepressants we have now are based on serendipitous discoveries from six decades ago. Antidepressants act on monoamines (molecules also known as neurotransmitters). There is no approved antidepressant that's non-monoamine acting.
We think that focusing on these gene networks would provide novel treatments for depression. Since all of today's treatments for depression focus on monoamine pathways, they're very limited. Even though we have hundreds of molecules, they're all basically the same.
SA: And today’s antidepressants don’t help all people?
EN: Large clinical trials show that only about half, maybe fewer than half of all people with depression, are fully treated—meaning they get fully well with available treatments. It’s no surprise that the same range of patients that respond to one drug respond to the others because all of the drugs basically act in the same way. There's been this desperate need in the field to develop antidepressants with novel mechanisms for those who aren’t helped by available drugsand we think this is one approach to doing that.
SA: Is it also possible that you might be able to take a wholly new approach of making those at risk for depression more resilient so that they don't become depressed?
EN: Yes, absolutely. Another approach is to look at the resilient mice in this study and ask: Can we identify genes that control resilience and then can we design still additional medications to boost resilience as a novel approach to antidepressant therapy. We think that that’s definitely possible. We have another study that's in the works now where we've looked at groups of genes that we've found through this type of analysis to be important for resilience and have demonstrated already the ability to manipulate these genes and make a mouse more resilient.
SA: These are only mouse models.
EN: This is a mouse study and one of the first things we need to do is to now validate these genes that have been found in depressed mice in post-mortem human brain tissue from depressed humans and that's work that we and others are also doing. We have another study that's under way employing very similar statistical approaches on human brain tissue, which we think is essential. The validity of this approach has been demonstrated by an ongoing clinical trial for depression at Mount Sinai: our clinical colleagues are testing in humans a molecule that was first shown to boost resilience in mouse models based on our gene expression data. Preliminary data are encouraging although far more work is needed to validate this finding.
SA: How would you describe your approach as being different from early-stage development for neurological drugs?
EN: First of all, very few companies are still in the psychiatry space. There is a desperate need because psychiatric disorders are among the most impactful on humanity and it's a tragedy that drug companies are not doing this. As far as drug development, almost all drug discovery efforts thus far have focused on candidate genes one at a time—in other words, they are not looking at all 20,000 genes at once and seeing which are the most important, but just basically guessing based on limited information about whether gene “A,” “B” or “C” might be interesting and then trying to develop something using that gene or its pathway. We think that we and others have articulated a fundamentally broader approach to drug discovery to really look at all genes in total and see which ones are the most important and then target those. I think that drug companies will start to do that pretty soon and that that will represent a major advance for the field, but we're still in very early stages.
(Other researchers on the Neuron paper (not all from Mt. Sinai) were: Rosemary C. Bagot, Hannah M. Cates, Immanuel Purushothaman, Zachary S. Lorsch, Deena M. Walker, Junshi Wang, Xiaojie Huang, Oliver M. Schlüter, Ian Maze, Catherine J. Peña, Elizabeth A. Heller, Orna Issler, Minghui Wang, Won-min Song, Jason. L. Stein, Xiaochuan Liu, Marie A. Doyle, Kimberly N. Scobie, Hao Sheng Sun, Rachael L. Neve, Daniel Geschwind, Yan Dong, Li Shen and Bin Zhang.)