This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
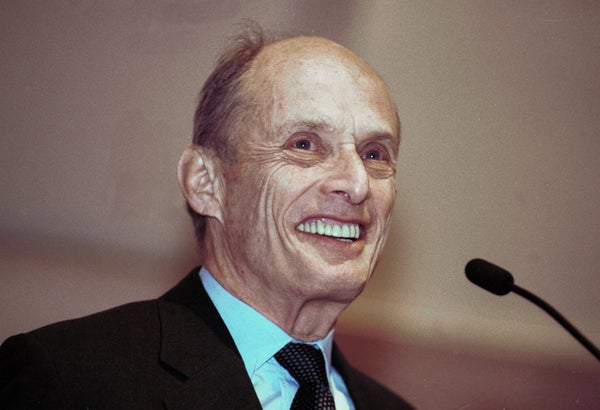
Editor’s Note: Nobel laureate Paul Greengard, who deepened science’s understanding of how neurons communicate, died April 13 at age 93. Greengard, who continued to work in his lab at Rockefeller University into his 10th decade, had spoken to Scientific American in December 2015 about ongoing research that related to Alzheimer’s, depression and Parkinson’s.
Paul Greengard has been busy. In August he co-authored a paper on molecules that appear to regulate genes that might protect against Parkinson’s. That same month he took the lead on another paper that describes a protein that plays a key role in producing the toxic peptide implicated in Alzheimer’s disease. He followed that up in September with a study laying out evidence for what could become a new class of antidepressants. On Friday, he will pause for a few hours as he celebrates his 90th birthday.
Greengard has maintained this same unwavering focus throughout his career. After working from 1959 to 1967 at the pharmaceutical company Geigy, he decided he could do more science—and even more drug development—in academia.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
At Albert Einstein College of Medicine and later at Yale University, he set about tracing the cellular pathways activated by dozens of signaling molecules called neurotransmitters. Since the early 1980s, about the time he moved to Rockefeller, he has used the knowledge gained from this basic research—discoveries that led to a Nobel Prize in 2000—to look for proteins and molecular pathways that might be targeted by pharmaceuticals for both psychiatric and neurodegenerative disorders. He also founded a company that now has an anti-schizophrenia drug in a late-stage clinical trial.
I met with Greengard recently in his office overlooking the East River, its walls adorned with giant wooden sculptures crafted by his wife, the noted artist Ursula von Rydingsvard. “She’s more well known than I am,” Greengard says. As he reaches nonagenarian status, the head of the 66-member lab at Rockefeller, one of the institution’s largest, has no intention of slowing down from his “six-and-a-half-day” work schedule. He talked to me last week about what he’s been up to recently.
[An edited transcript of the interview follows]
You’ve published a lot of papers this year. Has this been a really active year for you?
The number of publications is probably higher than average
Would you say this is the same number of papers you were publishing 10, 20, 30 years ago?
I think so, yes
It seems like what you've done at Rockefeller is built on some of the initial work that you did on neurotransmitters, mainly at other institutions, to look for the underlying causes of neurodegenerative diseases and mental illness.
That's fairly accurate. I would formulate it slightly differently.
The first part of my career was dedicated to understanding the mechanisms by which nerve cells communicate with each other. At the time I started my career, it was thought that when a neurotransmitter is released from one nerve cell, it activates an ion channel on another nerve cell. This turned out to be true but it turned out to be true primarily for the excitatory neurotransmitter glutamate and the inhibitory one GABA.
The major contribution of my research was to show that the situation is far more complicated. What you can call fast synaptic transmission—the transmission of the neurotransmitters glutamate and GABA, which was known when I started my work—can be thought of as the hardware of the brain.
What we did was to look at a large number of neurotransmitters, probably 100 neurotransmitters that worked through what we called slow synaptic transmission. Slow synaptic transmission activates receptors on the receiving nerve cells that then cause changes in chemicals known as second messengers, a whole internal signal transduction pathway within the cell that might be thought of as the brain’s software. It is now known that the vast majority of signaling in the brain is what we today call slow synaptic transmission.
Had you always intended to move beyond that?
I was always interested in the molecular basis of diseases and my first job after my postdoctoral training was in a pharmaceutical company. I was there for eight years. Then I decided that I could do more in the way of drug development in academia than I could in a pharmaceutical company.
Why?
It was mainly the bureaucracy, the gigantic size. Everything was run by committees. You couldn't start a program without getting approval of a committee and so it was an endless task to try to persuade people to agree to what I wanted to do.
So you worked on these signaling pathways for many years and then decided to look at specific diseases?
About the time I moved from Yale to Rockefeller—plus or minus five years—I felt we knew enough about these slow-signaling pathways that we could start asking meaningful questions, answerable questions, about the etiology of various neurological and psychiatric diseases and about the mechanisms by which the drugs used to treat those diseases achieve their molecular action.
And so we've worked on two neurodegenerative disorders for many years, Alzheimer's and Parkinson's, and two psychiatric disorders, major depressive disorder and schizophrenia. And what we're working on now is largely Parkinson’s, Alzheimer’s and depression. I did start a company [Intra-Cellular Therapies, New York] to work on schizophrenia with two other founders and that company has been very successful so far. We have a fantastic anti-schizophrenia drug that's now in late-stage clinical trials and the results look very, very positive. All the psychiatrists who have been studying this say there's never been a drug like it.
How is your drug different than the ones on the market?
I can explain it in a way where you can see where ours is coming from. There are eight or 10 different anti-schizophrenia drugs on the market that are very good and they all affect the positive symptoms of schizophrenia (delusions, hallucinations and disordered thinking) and none of them affect the negative symptoms (a lack of emotion, motivation and pleasure and a difficulty in communicating).
They all have different side effects so my reading was that if we were to look at the 10 drugs and see which pathways were common to the different classes of anti-schizophrenia drugs and assume that's the therapeutic pathway and we look at the signaling pathways that were specific to each drug that were different from the other drugs, that would equate to the drug’s toxicity. So if we then concentrate on finding drugs that emphasize that one common pathway without affecting the other pathways, then we might be able to get a drug which is therapeutically active without side effects. So that was the rationale, and the drug we developed is very interesting.
Things are going very well because this drug we now have is very successful with the positive symptoms of schizophrenia but it seems to be devoid of toxicity. But what was unanticipated was that these drugs also seem to be very effective in dealing with the negative symptoms. Doctors said they gave this drug to patients who had been sitting in a catatonic trance for 10 years and that within one month the patients got up and started helping other patients.
What about Alzheimer’s?
In Alzheimer’s there’s a pathological process that leads to formation of a toxic peptide called beta amyloid. So we’re doing studies on the metabolism of betaamyloid. Many laboratories, including our own, were focusing for years on the synthesis of beta amyloid, using the idea that you might have too much beta amyloid because your brain is making too much, but the studies from several laboratories now suggest that maybe the brain has a high level of beta amyloid because there's a decreased breakdown of the peptide.
So we began to study the metabolism of beta amyloid and found in fact that the breakdown of beta amyloid is very sensitive to changes in the brain and we've been working on a signaling pathway which activates the breakdown. We're now looking for drugs that interact with it.
You’ve also worked on ways to inhibit the synthesis of beta amyloid, which provides another approach to drug development.
Yes, we have been studying a protein called GSAP that causes increased synthesis of beta amyloid by activating an enzyme, called gamma secretase.
Are you still working on this project?
Yes. Right now we're looking at the mechanism by which GSAP regulates the level of beta amyloid.
Some of the drugs called gamma secretase inhibitors that pharmaceutical companies have tested have run into difficulties.
Gamma secretase interacts with dozens of other molecules so the goal has been to try to find inhibitors that prevent formation of beta amyloid without inhibiting some of these other pathways. There have been a number of studies where people have taken gamma secretase inhibitors and put them into patients and ended up with toxicity, which was all predictable in advance because they didn't avoid these other pathways.
In fact, you probably know that some people have said gamma secretase inhibitors are dead.
They've made those kinds of pronouncements. And they are wrong. I pronounce these pronouncements incorrect. Selective gamma secretase inhibitors are not dead.
Dopamine as a neurotransmitter was something you probably turned to fairly quickly right when you started looking for drug targets.
It was obviously one of the most interesting neurotransmitters. We knew where in the brain it worked, and the fact that it was involved in both Parkinson’s and schizophrenia. Basically all of the anti- schizophrenia drugs have a component of dopamine receptor antagonism. Antagonizing dopamine is a way to treat schizophrenia. Activating dopamine is also a way to treat Parkinson's. So there were two diseases that we were interested in and it was clear that that was a good neurotransmitter choice.
You published a paper recently that looked at pathways involved in Parkinson’s disease.
We collaborated with the laboratory of Nat Heintz, who is a professor at Rockefeller. We developed a technique called bacTrap that records the genetic messages being translated into proteins so that we were able to look at all of these messages in the cells that die in Parkinson's and distinguish them from cells that survive. We were able to find proteins that were master regulators of a lot of genes in both the cells that lived and those that died. That’s what the paper we published in recently in Nature Neuroscience was about. It gave us a whole molecular pathway that’s like a highway. I'm very optimistic that we'll be able to get to the beginning of that highway where the cell death process starts. It might be possible to intervene with a drug anywhere along that pathway. (Scientific American is part of Nature Publishing Group.)
Depression—let's get to depression.
Marc Flajolet and Per Svenningsson, members of our research group, found a protein, p11, that binds to three of the receptors for serotonin (a neurotransmitter that has an impact on mood.) So this was very exciting because the whole idea of this research was maybe there is some regulator that determines whether we're depressed or not depressed.
What we found is that p11 in the nerve cell results in more serotonin receptors being recruited to the cell surface. It turns out that p11 is highly concentrated in one cell type in each of several regions of the brain. You can think of those p11 cells as the master coordinators controlling the communication amongst all the cells in these areas. We’re doing several different projects to understand how p11 is controlling the function of several regions of the brain. The data are now overwhelming that the level of p11 determines whether the animal is depressed or not. We also found that p11 interacts with glutamate receptors, which are also linked to depression.
Switching gears, did you find the basic research in the early part of your career more interesting or the applied research later on?
They both give me great gratification but sort of different types of gratification. When I began studying slow signal transduction in the brain, people didn't accept the concept, for the most part. But, for some reason, I never doubted it and now there's some 3,000 laboratories working on signal transduction in the brain.
The work on disease pathways and how to modulate them—did that produce a different kind of gratification?
Yes, because of the practical aspects. It's really a different kind of pleasure that you've done something that will probably help people. For example, this schizophrenia drug we have, it makes me really, really happy because it seems that the treatment for schizophrenia will tremendously be changed by our new drug.
After all these years, is there a concise way that you can think of to sum up your work?
We are our signaling pathways.
We can't dissociate ourselves from our signaling pathways That's how all cells work: nerve cells and liver cells and every other kind of cell. The cells receive information through receptors. Those pathways that have evolved inside cells tell us what to do. So the knowledge of these pathways and all the chemical steps in them provide a large number of targets for drug development that would not have been available before.
You are intensely involved with your work and you’ve always been so. When you got the Nobel Prize, were you worried that it could become a distraction to doing the things that you wanted to do?
It seems there are two ways that people respond to winning a Nobel Prize and nothing in the middle. It seems that there are people who convert their Nobel Prize into being a president of a university or a head of a foundation and there are others who work harder at their science. I can give you examples of each. I happen to be in the latter group. I just love doing my work so much I have no interest in running an institute and determining which of the people under me should get more support for their work.
When you got your Nobel Prize, why did you decide to devote the money for a prize for women in the biomedical sciences?
Because I'd seen a great deal of discrimination against women. And that bothered me.
Do you think discrimination is there to the same extent?
No. I think people are much more aware. When I was a kid, many men and women believed that women were intellectually inferior to men. And then at some point, people started questioning it.
Did you find yourself part of the thinking of that generation as well?
I think I was as much a victim of the culture of the time. I mean I think if you'd asked me when I was 18 whether women are intellectually equal to men I probably would have said no. Part of it is women weren't doing math and science so I think I had that bigotry. It didn't take long for me to realize I was wrong. It's taken some people longer.
What made you realize that?
I have a mind where you question everything. When you hear women are inferior to men, you start questioning whether that's really true. You see a brilliant woman and you think maybe that idea is not right. I think people who become scientists have more open minds than most people do.. It wasn't hard for me to realize that I was the victim of cultural bias as it existed. I think things are a lot better now. I'm often in groups of male scientists where we are talking about how to get more women appointments at Rockefeller.
Do you still work as much as you did? Some people at the age of 90 want to still work but begin to lay off a bit.
I don't want to lay off. I get great joy out of my work. I have a wonderful group of younger colleagues and there are always extremely exciting things happening in the lab, which totally get to me. There are other things I enjoy but most of my family are like I am—they love their work.
Our family is very attached to each other. I would not miss some function with the family, a holiday or whatever.. But I go to the theater less often than I used to because I'm more and more involved in my work.
The work seems more demanding because of the nature of the work and not your energy? You still seem to have a lot of energy.
I think that's true. Because we've opened up these different avenues, there are more exciting questions that we can ask and answer now than we could, say, 30 years ago.
Would you ever consider retiring?
If I felt I was not capable of functioning efficiently, I would.
But as long as you are, you want to work at what you are doing for the rest of your life?
I do. It’s much more fun understanding the brain than doing a crossword puzzle. It’s the same kind of cognitive challenge, but it's much more fun and you feel you're doing something worthwhile.
Are there still big questions you’d like to get around to answering?
As long as I’m staying in brain science, I can't imagine trying to find another paradigm. I think the paradigm we found, the signaling pathways, provides such an enormous challenge to achieve an understanding of the basis of every neurological and psychiatric disorder and an understanding of how to treat those disorders and develop drugs that can be even better for the treatment of these disorders. That’s a pretty large task.